How To Diagnose and Treat Metabolic Syndrome
About 1 in 3 adults in the US experience metabolic syndrome. It affects millions of people, and is considered a serious health problem because it can increase your risk of heart disease, stroke, and developing diabetes.
In this article, we will explore what metabolic syndrome is, its symptoms, how metabolic syndrome is typically diagnosed & and some common risk factors. We will also answer some frequently asked questions about treatment for metabolic syndrome.
Understanding metabolic syndrome is important to maintaining your overall health and well-being, so let’s explore this important topic.
What is Metabolic Syndrome?
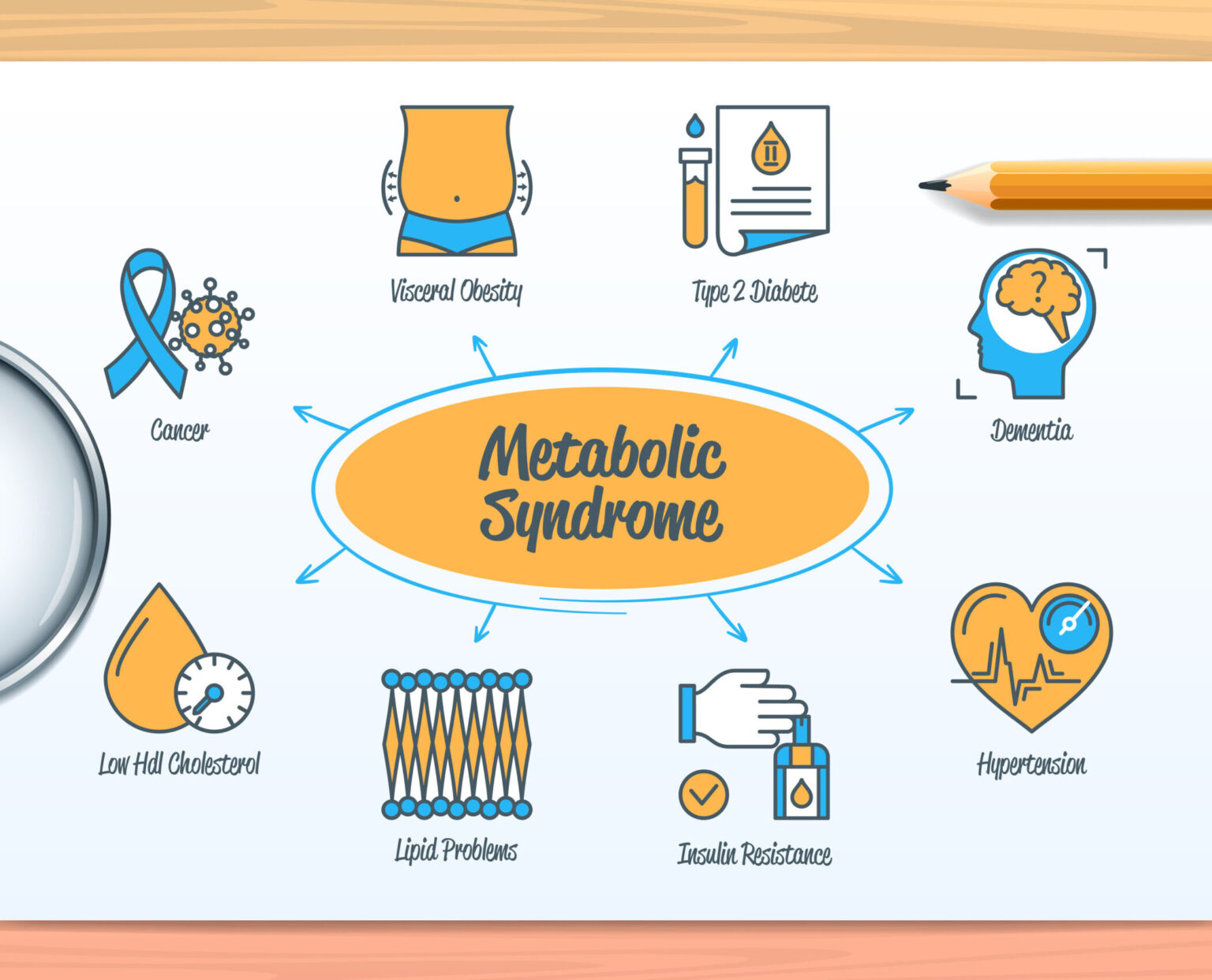
Metabolic syndrome is a way to describe a group of conditions that occur simultaneously, increasing the risk of cardiovascular disease, stroke, and diabetes. It is also known as insulin resistance syndrome.
Diagnostic Criteria for Metabolic Syndrome
The following are the conditions that correlate with metabolic syndrome:
- High blood pressure: Your blood pressure is considered elevated when it is regularly over the 130/85 mmHg mark.
- High blood sugar: Fasting blood sugar levels are considered high if they are consistently above 100 mg/dL.
- High triglyceride levels: According to the National Library of Medicine, Triglycerides are a type of fat found in the blood. They are considered high if they are consistently above 150 mg/dL.
- Genetics: Some people may have a genetic tendency to develop metabolic syndrome due to their genetic makeup. HDL (high-density lipoprotein) is known as the “good” cholesterol because it helps remove LDL (low-density lipoprotein) or “bad” cholesterol from the bloodstream. HDL is considered low if it is consistently below 40 mg/dL in men or below 50 mg/dL in women.
- Excess abdominal fat: The measurement of waist circumference is used to determine excess abdominal fat. Men with a waist circumference of 40 inches or more and women with a waist circumference of 35 inches or more are considered to have excess abdominal fat.
To be diagnosed with metabolic syndrome, a person must meet the criteria and have at least three of the above correlating conditions. If left untreated, these conditions can lead to serious health problems. Therefore, it is important to speak with your healthcare provider to manage and treat the symptoms of insulin resistance.
What causes metabolic syndrome?
It is unclear what the root causes of metabolic syndrome are, but it has been suggested that this condition is the result of a blend of both genetic and environmental influences. It appears that certain individuals may be born with an inherent susceptibility to developing metabolic syndrome, and the disorder is more prevalent among elderly people.
Metabolic Syndrome Risk Factors:
Factors that may contribute to the development of metabolic syndrome include:
- Insulin resistance: This occurs when the body’s cells become resistant to the effects of insulin, a hormone that regulates blood sugar levels.
- Obesity & weight gain: Excess weight & weight gain, especially around the waistline, can increase your risk.
- Inactivity: Lack of physical activity can contribute to insulin resistance and obesity.
- Genetics: Some people may be genetically predisposed to developing metabolic syndrome.
- Age: Metabolic syndrome is much more common in older adults.
- Smoking: Smoking can contribute to insulin resistance and other factors that increase the risk of metabolic syndrome.
- Poor diet: A diet high in saturated fats, trans fats, and sugar can increase the risk of insulin resistance and obesity.
- Sleep apnea: Sleep apnea is a condition in which breathing stops and starts during sleep. This is a risk factor.

Metabolic Syndrome Treatments
Conventional medicine treatments for metabolic syndrome typically involve managing individual risk factors and symptoms, such as blood pressure, blood sugar, or cholesterol levels, with medications. LifeStream’s metabolic syndrome treatment program offers an alternative: a comprehensive, personalized approach to addressing the underlying root causes of insulin resistance syndrome while improving overall health and wellbeing.
Our holistic medicine clinics take an evidence-based and patient-centered approach to healthcare. We seek to identify and treat the underlying causes of disease, rather than simply managing your symptoms.
Our expert functional medicine doctors consider each patient’s unique genetics, environment, lifestyle, and medical history when creating a personalized treatment plan for you.
LifeStream Treatment Highlights
Features of our metabolic syndrome treatment program, include but not limited to:
Health coaching:
Dietary changes are essential to treating metabolic syndrome and supporting healthy weight loss.
Nutritional supplements:
Nutritional supplements may be recommended to address specific nutrient deficiencies or support optimal metabolic function.
Hormone balancing:
Testing for hormonal imbalances and implementing hormone-balancing therapies such as bio-identical hormone replacement therapy (BHRT).
Gut health:
The health of the gut microbiome is closely linked to metabolic function.
Medical Weight Loss:
LifeStream’s medical weight loss program can help you achieve rapid fat loss and reach your goals with effective medications like Semaglutide.
Frequently Asked Questions
Insulin resistance is a condition in which the body's cells become less responsive to the hormone insulin, which is produced by the pancreas. Insulin is responsible for regulating blood sugar levels by enabling glucose to enter cells and be used for energy. In insulin resistance, the body's cells are unable to effectively use insulin, which leads to higher levels of glucose in the bloodstream. As a result, the pancreas must produce more insulin to maintain normal blood sugar levels.
The exact cause of insulin resistance is not fully understood, but it is believed to be the result of a combination of genetic and lifestyle factors. Some of the main factors that may contribute to insulin resistance include:
- Genetics: Some people may be genetically predisposed to insulin resistance.
- Obesity: Excess weight, especially around the abdomen, is strongly associated with insulin resistance.
- Sedentary lifestyle: Lack of physical activity can contribute to insulin resistance.
- Poor diet: A diet high in processed foods, refined carbohydrates, and saturated fats may increase the risk of insulin resistance.
- Sleep disturbances: Lack of sleep or poor sleep quality may increase insulin resistance.
- Chronic inflammation: Chronic inflammation, which can be caused by factors such as smoking, stress, and certain medical conditions, may contribute to insulin resistance.
- Hormonal imbalances: Imbalances in hormones such as cortisol, estrogen, and testosterone can affect insulin sensitivity.
It's important to note that while these factors can contribute to insulin resistance, not everyone who is overweight, inactive, or has a poor diet will develop the condition. Similarly, some people who are lean and physically active may still develop insulin resistance.
While metabolic syndrome is not directly responsible for weight gain, it can contribute to weight gain over time. One of the defining features of metabolic syndrome is insulin resistance, which can lead to high blood sugar levels and weight gain. When the body becomes resistant to insulin, it has difficulty using glucose for energy, which can lead to an increase in hunger and cravings for high-carbohydrate, high-calorie foods.
Additionally, metabolic syndrome can affect the body's ability to metabolize and store fat, leading to increased abdominal fat and weight gain. This is because insulin resistance can cause the body to store excess glucose as fat, especially around the midsection.
Therefore, while metabolic syndrome itself does not cause weight gain, it can contribute to it indirectly through its effects on insulin resistance and fat metabolism.
The most common metabolic disorder is diabetes mellitus. This is a chronic condition that affects how the body processes blood sugar (glucose), leading to high levels of glucose in the bloodstream. There are two main types of diabetes: type 1, which is typically diagnosed in childhood or young adulthood and is caused by the body's immune system attacking and destroying the cells in the pancreas that produce insulin; and type 2, which is more common and is usually diagnosed in adulthood, although it is becoming more common in children and teens as well.
Other common metabolic disorders include metabolic syndrome, hypothyroidism, hyperthyroidism, and hyperlipidemia.
The specific test results used to diagnose a metabolic disorder will depend on the type of disorder suspected. Generally, a provider will perform a physical exam, take a medical history, and order laboratory tests to assess the functioning of various metabolic pathways and organs.
Common tests used to diagnose metabolic disorders include:
- Blood tests: Blood tests are used to measure levels of specific chemicals and enzymes in the blood. Elevated or reduced levels of certain enzymes can indicate a metabolic disorder.
- Urine tests: Urine tests can measure levels of specific chemicals and byproducts of metabolism. Abnormal levels of these substances can indicate a metabolic disorder.
- Genetic testing: Genetic testing can identify specific genetic mutations that cause metabolic disorders.
- Imaging tests: Imaging tests, such as X-rays, computed tomography (CT) scans, and magnetic resonance imaging (MRI) can help detect abnormalities in organs and tissues that may indicate a metabolic disorder.
- Biopsy: A biopsy involves taking a small sample of tissue from an affected organ, which can be examined under a microscope to identify any metabolic abnormalities.
Healthcare Providers may use other diagnostic tools and advanced testing to assess the impact of a metabolic disorder on the heart and other organs.
While metabolic syndrome is a complex condition, it is possible to reverse it through lifestyle changes. These changes may include:
- Losing weight: Achieving and maintaining a healthy weight is one of the most effective ways to reverse metabolic syndrome.
- Increased physical activity: Engaging in regular physical activity can help make your body more sensitive to insulin, decrease your blood pressure, and reduce the amount of cholesterol in your body.
- Insulin Resistance: The body's cells can become less responsive to insulin, a hormone that manages the amount of glucose in the blood, which is known as insulin resistance.Metabolic syndrome's cause is uncertain, however it is assumed to be the result of a mix of both genetic and environmental elements.
- Eating a healthy diet: Focus on a diet rich in whole, nutrient-dense foods such as fruits, vegetables, whole grains, lean proteins, and healthy fats. Avoid processed and high-sugar foods.
- Quitting smoking: Smoking can increase insulin resistance and worsen metabolic syndrome. Quitting smoking can help improve your overall health.
- Managing stress: Chronic stress can increase cortisol levels, which can contribute to metabolic syndrome. Try stress-reducing techniques such as meditation, yoga, or deep breathing exercises.
It's important to work with your healthcare provider to develop a plan that's tailored to your individual needs and health status.
Many patients find success with a combination of aerobic and resistance exercise.
Aerobic exercise can help improve cardiovascular health and decrease body fat, which are two key components of metabolic syndrome. Examples of aerobic exercises include walking, jogging, cycling, swimming, and dancing.
Resistance exercise, such as weightlifting, can help increase muscle mass and improve insulin sensitivity, which can help regulate blood sugar levels and decrease the risk of developing type 2 diabetes.
Combining both types of exercise can be highly beneficial for individuals with metabolic syndrome. It is always recommended to consult with your healthcare professional before starting a new exercise regimen.
While there are multiple organs involved in metabolic syndrome, it primarily affects the body's metabolism and can have an impact on several organs, including the liver, pancreas, and heart.
In metabolic syndrome, the body's ability to use insulin effectively to process glucose (sugar) is impaired. This leads to high blood sugar levels, which can damage organs throughout the body, including the heart, kidneys, eyes, and nerves. The liver can also become insulin resistant, leading to a buildup of fat in the liver and potentially leading to non-alcoholic fatty liver disease.


